Researchers have revealed another benefit of using whole genome and transcriptome sequencing to inform cancer patient care: the detection of gene fusions that are treatable with currently available therapeutics.
The study, published in Clinical Cancer Research, was led by BC Cancer Medical Oncologist Dr. Jonathan Loree as part of BC Cancer’s Personalized OncoGenomics (POG) program—a precision oncology initiative that performs whole genome and transcriptome sequencing to identify targetable genetic alterations in patients with metastatic disease.
To investigate the potential advantage of a whole-genome sequencing approach over standard target-based panel testing—and specifically its ability to detect gene fusions—researchers analyzed the DNA and RNA sequencing data from the first 570 patients to be enrolled in the program.
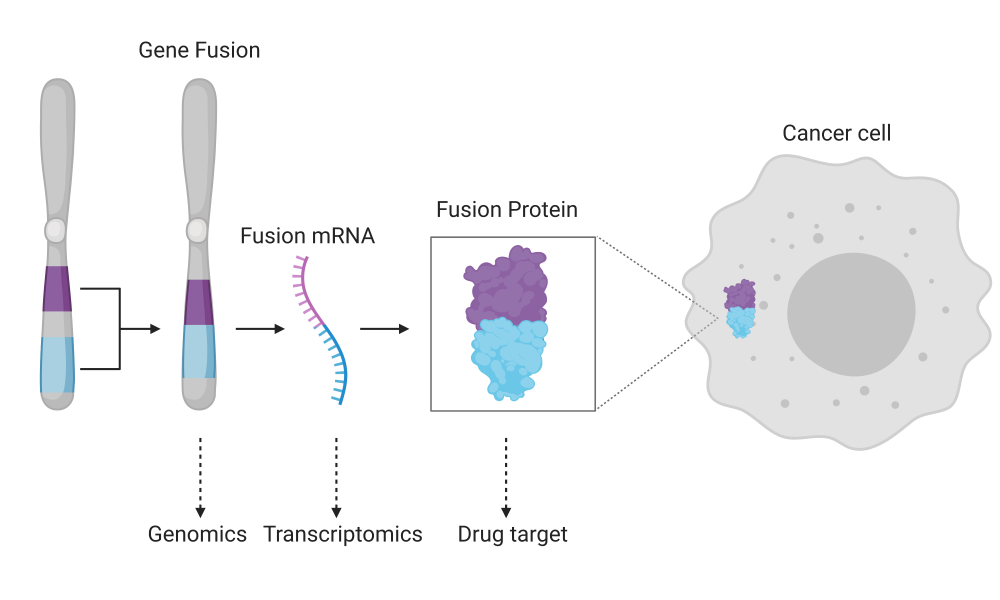
Gene fusions occur when genomic rearrangements lead to two previously independent genes becoming fused together. This can result in a change to the normal growth and metabolism of cell through the production of unusual, malfunctioning or non-functioning proteins. It can also lead to a gene being expressed more frequently than usual if it becomes fused to one that has a higher level of expression. In this way, gene fusions can lead to cancer and encourage its growth and resistance to therapies. Some of these fusions, such as those involving the fused NRG1 gene in pancreatic ductal adenocarcinoma, for example, are treatable, as described in another POG study.
“Our aim was to determine the true prevalence of gene fusion events. One of the challenges of identifying fusions is that you kind of need to know that they’re there in order to look for them; you need to know who the partners are in that fusion,” says Dr. Loree. “We wanted to see if we could use the techniques from the POG program to try to get a better sense of the fusions that we didn’t know were there before, and try to use this to discover more fusions that are potentially treatable.”
The study cohort of 570 advanced-stage cancer patients included 25 different cancers and 18 organ groups, allowing for the analysis of fusion events across tumour types. Ninety-five per cent of the patients were found to have at least one gene fusion, and bioinformatic analysis uncovered 81 unique gene fusions by genome sequencing and 111 by transcriptome analysis that were recurrent in the cohort. Recurrent fusions were found in 30 per cent of the patients, which was much higher than anticipated.
“We decided to focus on the recurrent fusions because it is actually quite challenging to determine whether or not a fusion has clinical significance,” says Dr. Loree. “But if we see the same genetic event happening in more than one patient, then we have a higher level of confidence that it is actually something that is functionally significant.”
Commercial panel tests for gene fusions are available and routinely used in the clinic. The researchers investigated the robustness of these tests in comparison with whole genome and transcriptome analysis and found that the commercially available tests were only able to detect less than 10 per cent of the gene fusions that have been identified through the POG program using whole genome analysis.
“This study gives us a better sense of how many patients might have one of these fusions, and the scope of [these fusions] suggests this is something we really need to pay attention to,” says Dr. Loree.
Importantly, the study also led to the identification of previously uncharacterized gene fusions, contributing to the body of knowledge and providing hypotheses for the development of novel therapies.
“Our study highlights the benefits of the detailed genomic sequencing performed by POG. By identifying new fusions, we can potentially unveil new treatment targets for cancer patients,” says Dr. Erica Tsang, former BC Cancer Medical Oncology Resident and lead author on the study. “Whole genome sequencing helps in the discovery process, and future studies may help to clarify when to use this type of detailed genetic sequencing compared to the standard commercially available panel. Each approach has its own benefits and drawbacks, and we continue to learn how to best use these technologies to improve our care for patients with cancer.”
Moving forward, the research group aims to gain a better understanding of the novel gene fusions identified in this study and their role in cancer development and progression, and to investigate novel therapies that target them.
“On a larger scale, we also hope to learn more about the role of using these genomic technologies as they evolve over time,” says Dr. Tsang. “We are very fortunate in B.C. to have a superb team of bioinformaticians, clinicians, and researchers who all work together to improve the quality of life and care for individuals living with cancer.”
Learn more about the Personalized OncoGenomics program
Erica S. Tsang, Cameron J. Grisdale, Erin Pleasance, James T. Topham, Karen Mungall, Caralyn Reisle, Caleb Choo, Marcus Carreira, Reanne Bowlby, Joanna M. Karasinska, Daniel MacMillan, Laura M. Williamson, Eric Chuah, Richard A. Moore, Andrew J. Mungall, Yongjun Zhao, Basile Tessier-Cloutier, Tony Ng, Sophie Sun, Howard J. Lim, David F. Schaeffer, Daniel J. Renouf, Stephen Yip, Janessa Laskin, Marco A. Marra, Steven J.M. Jones, Jonathan Loree. 2020. Uncovering clinically relevant gene fusions with integrated genomic and transcriptomic profiling of metastatic cancers. Clinical Cancer Research. Online ahead of print.
This study would not have been possible without the participation of the patients enrolled in the POG program and the generous support of the BC Cancer Foundation. Funding support was also provided by Michael Smith Health Professional Investigator Awards to Drs. Renouf and Loree, the VCHRI Investigator Award to Dr. Schaeffer, GSC infrastructure investments from the Canada Foundation for Innovation and the Canada Research Chairs and the CIHR Foundation programs.