Science translational medicine, 2022
Evgin, Laura, Kottke, Tim, Tonne, Jason, Thompson, Jill, Huff, Amanda L, van Vloten, Jacob, Moore, Madelyn, Michael, Josefine, Driscoll, Christopher, Pulido, Jose, Swanson, Eric, Kennedy, Richard, Coffey, Matt, Loghmani, Houra, Sanchez-Perez, Luis, Olivier, Gloria, Harrington, Kevin, Pandha, Hardev, Melcher, Alan, Diaz, Rosa Maria, Vile, Richard G
Oncolytic viruses (OVs) encoding a variety of transgenes have been evaluated as therapeutic tools to increase the efficacy of chimeric antigen receptor (CAR)-modified T cells in the solid tumor microenvironment (TME). Here, using systemically delivered OVs and CAR T cells in immunocompetent mouse models, we have defined a mechanism by which OVs can potentiate CAR T cell efficacy against solid tumor models of melanoma and glioma. We show that stimulation of the native T cell receptor (TCR) with viral or virally encoded epitopes gives rise to enhanced proliferation, CAR-directed antitumor function, and distinct memory phenotypes. In vivo expansion of dual-specific (DS) CAR T cells was leveraged by in vitro preloading with oncolytic vesicular stomatitis virus (VSV) or reovirus, allowing for a further in vivo expansion and reactivation of T cells by homologous boosting. This treatment led to prolonged survival of mice with subcutaneous melanoma and intracranial glioma tumors. Human CD19 CAR T cells could also be expanded in vitro with TCR reactivity against viral or virally encoded antigens and was associated with greater CAR-directed cytokine production. Our data highlight the utility of combining OV and CAR T cell therapy and show that stimulation of the native TCR can be exploited to enhance CAR T cell activity and efficacy in mice.
Timothy Kottke, Jason Tonne, Laura Evgin, Christopher B Driscoll, Jacob van Vloten, Victoria A Jennings, Amanda L Huff, Brady Zell, Jill M Thompson, Phonphimon Wongthida, Jose Pulido, Matthew R Schuelke, Adel Samson, Peter Selby, Elizabeth Ilett, Mark McNiven, Lewis R Roberts, Mitesh J Borad, Hardev Pandha, Kevin Harrington, Alan Melcher, Richard G Vile
In our clinical trials of oncolytic vesicular stomatitis virus expressing interferon beta (VSV-IFNβ), several patients achieved initial responses followed by aggressive relapse. We show here that VSV-IFNβ-escape tumors predictably express a point-mutated CSDE1P5S form of the RNA-binding Cold Shock Domain-containing E1 protein, which promotes escape as an inhibitor of VSV replication by disrupting viral transcription. Given time, VSV-IFNβ evolves a compensatory mutation in the P/M Inter-Genic Region which rescues replication in CSDE1P5S cells. These data show that CSDE1 is a major cellular co-factor for VSV replication. However, CSDE1P5S also generates a neo-epitope recognized by non-tolerized T cells. We exploit this predictable neo-antigenesis to drive, and trap, tumors into an escape phenotype, which can be ambushed by vaccination against CSDE1P5S, preventing tumor escape. Combining frontline therapy with escape-targeting immunotherapy will be applicable across multiple therapies which drive tumor mutation/evolution and simultaneously generate novel, targetable immunopeptidomes associated with acquired treatment resistance.
Cancers, 2021
Evgin, Laura, Vile, Richard G
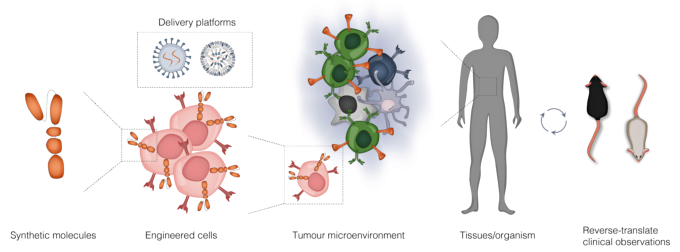
Oncolytic viruses (OVs) and adoptive T cell therapy (ACT) each possess direct tumour cytolytic capabilities, and their combination potentially seems like a match made in heaven to complement the strengths and weakness of each modality. While providing strong innate immune stimulation that can mobilize adaptive responses, the magnitude of anti-tumour T cell priming induced by OVs is often modest. Chimeric antigen receptor (CAR) modified T cells bypass conventional T cell education through introduction of a synthetic receptor; however, realization of their full therapeutic properties can be stunted by the heavily immune-suppressive nature of the tumour microenvironment (TME). Oncolytic viruses have thus been seen as a natural ally to overcome immunosuppressive mechanisms in the TME which limit CAR T cell infiltration and functionality. Engineering has further endowed viruses with the ability to express transgenes in situ to relieve T cell tumour-intrinsic resistance mechanisms and decorate the tumour with antigen to overcome antigen heterogeneity or loss. Despite this helpful remodeling of the tumour microenvironment, it has simultaneously become clear that not all virus induced effects are favourable for CAR T, begging the question whether viruses act as valets ushering CAR T into their active site, or vandals which cause chaos leading to both tumour and T cell death. Herein, we summarize recent studies combining these two therapeutic modalities and seek to place them within the broader context of viral T cell immunology which will help to overcome the current limitations of effective CAR T therapy to make the most of combinatorial strategies.
Molecular therapy : the journal of the American Society of Gene Therapy, 2020
Huff, Amanda L, Evgin, Laura, Thompson, Jill, Kottke, Tim, Driscoll, Christopher B, Tonne, Jason, Wongthida, Phonphimon, Schuelke, Matthew, Shim, Kevin G, Mer, Georges, Ramirez-Alvarado, Marina, Vile, Richard
Enhancing the immunogenicity of tumor-associated antigens would represent a major advance for anti-tumor vaccination strategies. Here, we investigated structure-directed antigen destabilization as a strategy to improve the degradation, immunogenic epitope presentation, and T cell activation against a vesicular stomatitis virus (VSV)-encoded tumor antigen. We used the crystal structure of the model antigen ovalbumin to identify charge-disrupting amino acid mutations that were predicted to decrease the stability of the protein. One mutation, OVA-C12R, significantly reduced the half-life of the protein and was preferentially degraded in a 26-S proteasomal-dependent manner. The destabilized ovalbumin protein exhibited enhanced presentation of the major histocompatibility complex (MHC) class I immunogenic epitope, SIINFEKL, on the surface of B16F10 cells or murine bone marrow-derived dendritic cells (BMDCs) in vitro. Enhanced presentation correlated with better recognition by cognate CD8 OT-I T cells as measured by activation, proliferation, and effector cytokine production. Finally, VSV encoding the degradation-prone antigen was better able to prime an antigen ovalbumin-specific CD8 T cell response in vivo without altering the anti-viral CD8 T cell response. Our studies highlight that not only is the choice of antigen in cancer vaccines of importance, but that emphasis should be placed on modifying antigen quality to ensure optimal priming of anti-tumor responses.
Neuro-oncology, 2020
Wongthida, Phonphimon, Schuelke, Matthew R, Driscoll, Christopher B, Kottke, Timothy, Thompson, Jill M, Tonne, Jason, Stone, Cathy, Huff, Amanda L, Wetmore, Cynthia, Davies, James A, Parker, Alan L, Evgin, Laura, Vile, Richard G
Diffuse midline glioma, formerly DIPG (diffuse intrinsic pontine glioma), is the deadliest pediatric brainstem tumor with median survival of less than one year. Here, we investigated (i) whether direct delivery of adenovirus-expressing cluster of differentiation (CD)40 ligand (Ad-CD40L) to brainstem tumors would induce immune-mediated tumor clearance and (ii) if so, whether therapy would be associated with a manageable toxicity due to immune-mediated inflammation in the brainstem.
Nature communications, 2020
Evgin, Laura, Huff, Amanda L, Wongthida, Phonphimon, Thompson, Jill, Kottke, Tim, Tonne, Jason, Schuelke, Matthew, Ayasoufi, Katayoun, Driscoll, Christopher B, Shim, Kevin G, Reynolds, Pierce, Monie, Dileep D, Johnson, Aaron J, Coffey, Matt, Young, Sarah L, Archer, Gary, Sampson, John, Pulido, Jose, Perez, Luis Sanchez, Vile, Richard
The application of adoptive T cell therapies, including those using chimeric antigen receptor (CAR)-modified T cells, to solid tumors requires combinatorial strategies to overcome immune suppression associated with the tumor microenvironment. Here we test whether the inflammatory nature of oncolytic viruses and their ability to remodel the tumor microenvironment may help to recruit and potentiate the functionality of CAR T cells. Contrary to our hypothesis, VSVmIFNβ infection is associated with attrition of murine EGFRvIII CAR T cells in a B16EGFRvIII model, despite inducing a robust proinflammatory shift in the chemokine profile. Mechanistically, type I interferon (IFN) expressed following infection promotes apoptosis, activation, and inhibitory receptor expression, and interferon-insensitive CAR T cells enable combinatorial therapy with VSVmIFNβ. Our study uncovers an unexpected mechanism of therapeutic interference, and prompts further investigation into the interaction between CAR T cells and oncolytic viruses to optimize combination therapy.
Molecular therapy oncolytics, 2020
Eckert, Elizabeth C, Nace, Rebecca A, Tonne, Jason M, Evgin, Laura, Vile, Richard G, Russell, Stephen J
Genetically modified vesicular stomatitis virus (VSV) is an attractive agent for cancer treatment due to rapid intratumoral replication and observed clinical responses. Although VSV selectively kills malignant cells and can boost antitumor immunity, limited induction of intratumoral immune infiltration remains a barrier to efficacy in some cancer models. Here we engineered the oncolytic VSV platform to encode the T cell chemokine CXCL9, which is known to mediate the recruitment of activated CD8{{sup}}+{{/sup}} cytotoxic T cells and CD4{{sup}}+{{/sup}} T helper cells, and demonstrates conserved protein function between mice and humans. Chemotactic activity of the virally encoded chemokine was confirmed . Intratumoral concentration of CXCL9 was shown to increase after VSV therapy in three different cancer models, but to a much greater degree after VSV-CXCL9 therapy as compared with VSV control viruses. Despite a steep chemokine gradient from the tumor to the bloodstream, tumor trafficking of adoptively transferred and endogenous T cells was not measurably increased following VSV-CXCL9 therapy. Our results indicate that oncolytic VSV infection promotes release of CXCL9 in the tumor microenvironment, but further boosting of the functional chemokine gradient through virus engineering has little incremental impact on intratumoral immune cell infiltration in mouse and human tumor models.
Nature communications, 2020
Driscoll, Christopher B, Schuelke, Matthew R, Kottke, Timothy, Thompson, Jill M, Wongthida, Phonphimon, Tonne, Jason M, Huff, Amanda L, Miller, Amber, Shim, Kevin G, Molan, Amy, Wetmore, Cynthia, Selby, Peter, Samson, Adel, Harrington, Kevin, Pandha, Hardev, Melcher, Alan, Pulido, Jose S, Harris, Reuben, Evgin, Laura, Vile, Richard G
APOBEC3B, an anti-viral cytidine deaminase which induces DNA mutations, has been implicated as a mediator of cancer evolution and therapeutic resistance. Mutational plasticity also drives generation of neoepitopes, which prime anti-tumor T cells. Here, we show that overexpression of APOBEC3B in tumors increases resistance to chemotherapy, but simultaneously heightens sensitivity to immune checkpoint blockade in a murine model of melanoma. However, in the vaccine setting, APOBEC3B-mediated mutations reproducibly generate heteroclitic neoepitopes in vaccine cells which activate de novo T cell responses. These cross react against parental, unmodified tumors and lead to a high rate of cures in both subcutaneous and intra-cranial tumor models. Heteroclitic Epitope Activated Therapy (HEAT) dispenses with the need to identify patient specific neoepitopes and tumor reactive T cells ex vivo. Thus, actively driving a high mutational load in tumor cell vaccines increases their immunogenicity to drive anti-tumor therapy in combination with immune checkpoint blockade.
Journal for immunotherapy of cancer, 2019
Schuelke, Matthew R, Wongthida, Phonphimon, Thompson, Jill, Kottke, Timothy, Driscoll, Christopher B, Huff, Amanda L, Shim, Kevin G, Coffey, Matt, Pulido, Jose, Evgin, Laura, Vile, Richard G
Immunotherapy has shown remarkable clinical promise in the treatment of various types of cancers. However, clinical benefits derive from a highly inflammatory mechanism of action. This presents unique challenges for use in pediatric brainstem tumors including diffuse intrinsic pontine glioma (DIPG), since treatment-related inflammation could cause catastrophic toxicity. Therefore, the goal of this study was to investigate whether inflammatory, immune-based therapies are likely to be too dangerous to pursue for the treatment of pediatric brainstem tumors.
Cancer immunology research, 2019
Evgin, Laura, Huff, Amanda L, Kottke, Timothy, Thompson, Jill, Molan, Amy M, Driscoll, Christopher B, Schuelke, Matthew, Shim, Kevin G, Wongthida, Phonphimon, Ilett, Elizabeth J, Smith, Karen Kaluza, Harris, Reuben S, Coffey, Matt, Pulido, Jose S, Pandha, Hardev, Selby, Peter J, Harrington, Kevin J, Melcher, Alan, Vile, Richard G
Antitumor T-cell responses raised by first-line therapies such as chemotherapy, radiation, tumor cell vaccines, and viroimmunotherapy tend to be weak, both quantitatively (low frequency) and qualitatively (low affinity). We show here that T cells that recognize tumor-associated antigens can directly kill tumor cells if used at high effector-to-target ratios. However, when these tumor-reactive T cells were present at suboptimal ratios, direct T-cell-mediated tumor cell killing was reduced and the ability of tumor cells to evolve away from a coapplied therapy (oncolytic or suicide gene therapy) was promoted. This T-cell-mediated increase in therapeutic resistance was associated with C to T transition mutations that are characteristic of APOBEC3 cytosine deaminase activity and was induced through a TNFα and protein kinase C-dependent pathway. Short hairpin RNA inhibition of endogenous APOBEC3 reduced rates of tumor escape from oncolytic virus or suicide gene therapy to those seen in the absence of antitumor T-cell coculture. Conversely, overexpression of human APOBEC3B in tumor cells enhanced escape from suicide gene therapy and oncolytic virus therapy both and Our data suggest that weak affinity or low frequency T-cell responses against tumor antigens may contribute to the ability of tumor cells to evolve away from first-line therapies. We conclude that immunotherapies need to be optimized as early as possible so that, if they do not kill the tumor completely, they do not promote treatment resistance.
Molecular therapy oncolytics, 2018
Huff, Amanda L, Wongthida, Phonphimon, Kottke, Timothy, Thompson, Jill M, Driscoll, Christopher B, Schuelke, Matthew, Shim, Kevin G, Harris, Reuben S, Molan, Amy, Pulido, Jose S, Selby, Peter J, Harrington, Kevin J, Melcher, Alan, Evgin, Laura, Vile, Richard G
Tumor cells frequently evade applied therapies through the accumulation of genomic mutations and rapid evolution. In the case of oncolytic virotherapy, understanding the mechanisms by which cancer cells develop resistance to infection and lysis is critical to the development of more effective viral-based platforms. Here, we identify APOBEC3 as an important factor that restricts the potency of oncolytic vesicular stomatitis virus (VSV). We show that VSV infection of B16 murine melanoma cells upregulated APOBEC3 in an IFN-β-dependent manner, which was responsible for the evolution of virus-resistant cell populations and suggested that APOBEC3 expression promoted the acquisition of a virus-resistant phenotype. Knockdown of APOBEC3 in B16 cells diminished their capacity to develop resistance to VSV infection and enhanced the therapeutic effect of VSV . Similarly, overexpression of human APOBEC3B promoted the acquisition of resistance to oncolytic VSV both and . Finally, we demonstrate that APOBEC3B expression had a direct effect on the fitness of VSV, an RNA virus that has not previously been identified as restricted by APOBEC3B. This research identifies APOBEC3 enzymes as key players to target in order to improve the efficacy of viral or broader nucleic acid-based therapeutic platforms.
Clinical cancer research : an official journal of the American Association for Cancer Research, 2018
Uusi-Kerttula, Hanni, Davies, James A, Thompson, Jill M, Wongthida, Phonphimon, Evgin, Laura, Shim, Kevin G, Bradshaw, Angela, Baker, Alexander T, Rizkallah, Pierre J, Jones, Rachel, Hanna, Louise, Hudson, Emma, Vile, Richard G, Chester, John D, Parker, Alan L
Virotherapies are maturing in the clinical setting. Adenoviruses (Ad) are excellent vectors for the manipulability and tolerance of transgenes. Poor tumor selectivity, off-target sequestration, and immune inactivation hamper clinical efficacy. We sought to completely redesign Ad5 into a refined, tumor-selective virotherapy targeted to αvβ6 integrin, which is expressed in a range of aggressively transformed epithelial cancers but nondetectable in healthy tissues. Ad5{{sub}}NULL{{/sub}}-A20 harbors mutations in each major capsid protein to preclude uptake via all native pathways. Tumor-tropism via αvβ6 targeting was achieved by genetic insertion of A20 peptide (NAVPNLRGDLQVLAQKVART) within the fiber knob protein. The vector's selectivity and was assessed. The tropism-ablating triple mutation completely blocked all native cell entry pathways of Ad5{{sub}}NULL{{/sub}}-A20 via coxsackie and adenovirus receptor (CAR), αvβ3/5 integrins, and coagulation factor 10 (FX). Ad5{{sub}}NULL{{/sub}}-A20 efficiently and selectively transduced αvβ6{{sup}}+{{/sup}} cell lines and primary clinical ascites-derived EOC , including in the presence of preexisting anti-Ad5 immunity. biodistribution of Ad5{{sub}}NULL{{/sub}}-A20 following systemic delivery in non-tumor-bearing mice was significantly reduced in all off-target organs, including a remarkable 10{{sup}}7{{/sup}}-fold reduced genome accumulation in the liver compared with Ad5. Tumor uptake, transgene expression, and efficacy were confirmed in a peritoneal SKOV3 xenograft model of human EOC, where oncolytic Ad5{{sub}}NULL{{/sub}}-A20-treated animals demonstrated significantly improved survival compared with those treated with oncolytic Ad5. Oncolytic Ad5{{sub}}NULL{{/sub}}-A20 virotherapies represent an excellent vector for local and systemic targeting of αvβ6-overexpressing cancers and exciting platforms for tumor-selective overexpression of therapeutic anticancer modalities, including immune checkpoint inhibitors. .
Journal for immunotherapy of cancer, 2018
Forbes, Neil S, Coffin, Robert S, Deng, Liang, Evgin, Laura, Fiering, Steve, Giacalone, Matthew, Gravekamp, Claudia, Gulley, James L, Gunn, Hal, Hoffman, Robert M, Kaur, Balveen, Liu, Ke, Lyerly, Herbert Kim, Marciscano, Ariel E, Moradian, Eddie, Ruppel, Sheryl, Saltzman, Daniel A, Tattersall, Peter J, Thorne, Steve, Vile, Richard G, Zhang, Halle Huihong, Zhou, Shibin, McFadden, Grant
In this White Paper, we discuss the current state of microbial cancer therapy. This paper resulted from a meeting ('Microbial Based Cancer Therapy') at the US National Cancer Institute in the summer of 2017. Here, we define 'Microbial Therapy' to include both oncolytic viral therapy and bacterial anticancer therapy. Both of these fields exploit tumor-specific infectious microbes to treat cancer, have similar mechanisms of action, and are facing similar challenges to commercialization. We designed this paper to nucleate this growing field of microbial therapeutics and increase interactions between researchers in it and related fields. The authors of this paper include many primary researchers in this field. In this paper, we discuss the potential, status and opportunities for microbial therapy as well as strategies attempted to date and important questions that need to be addressed. The main areas that we think will have the greatest impact are immune stimulation, control of efficacy, control of delivery, and safety. There is much excitement about the potential of this field to treat currently intractable cancer. Much of the potential exists because these therapies utilize unique mechanisms of action, difficult to achieve with other biological or small molecule drugs. By better understanding and controlling these mechanisms, we will create new therapies that will become integral components of cancer care.